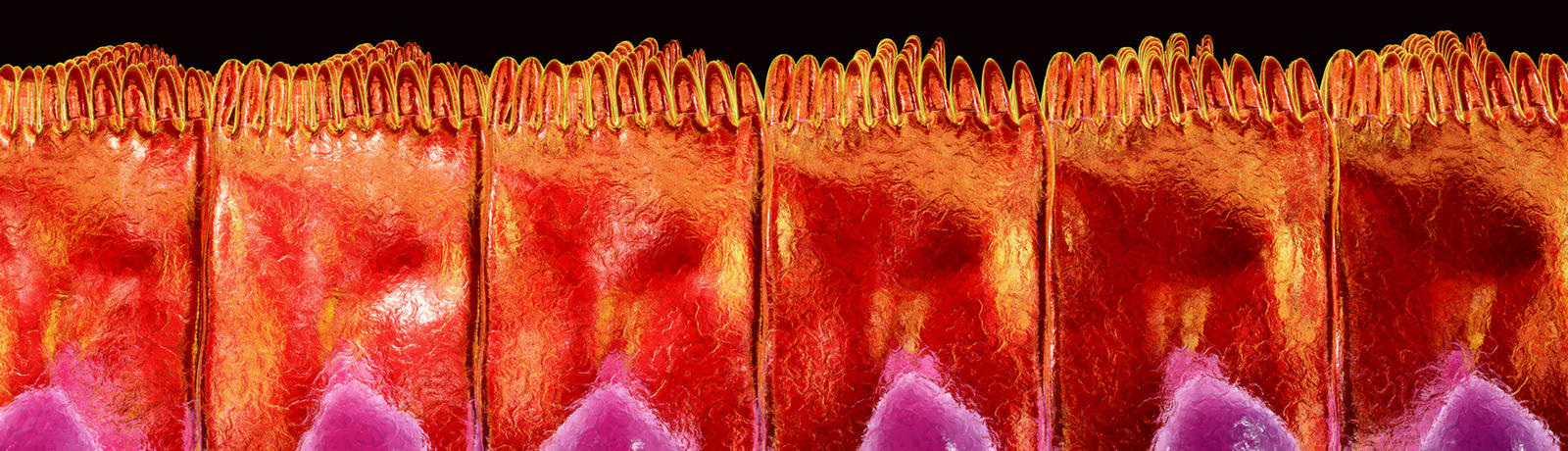
Our gut microbes have coevolved with us to form an intricate, dynamic, and mutually beneficial relationship.
How many microbes are in our gut?
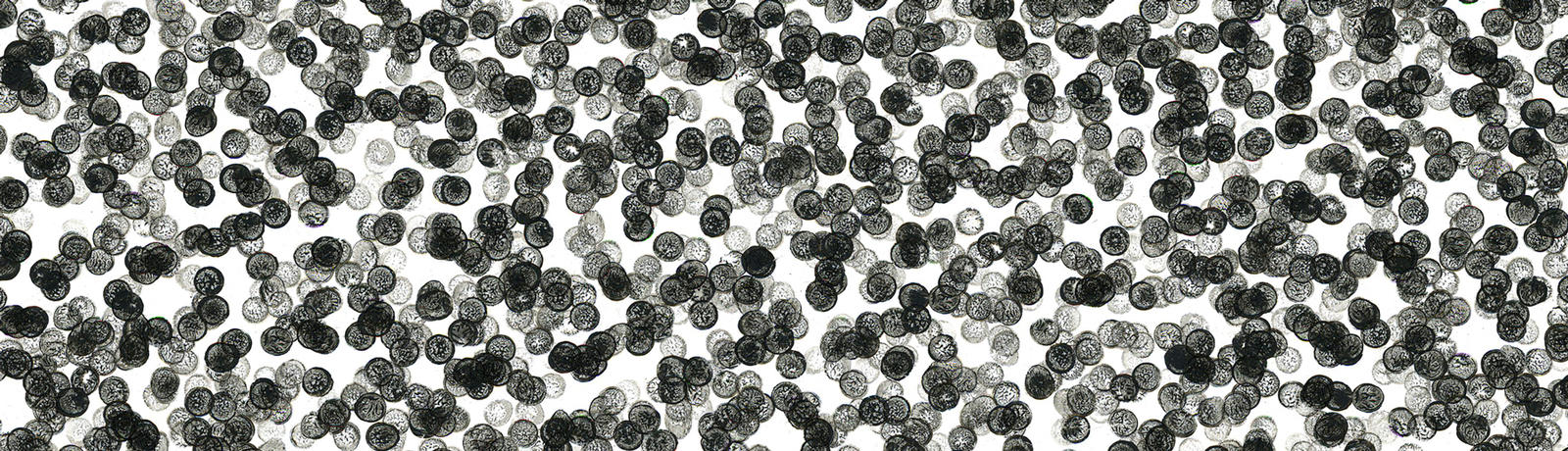
Scientists estimate that there are 39 trillion microbes living in the gut of a 154.3 lb. (70 kg) man, outnumbering the estimated 30 trillion cells in his body, weighing about 7 lb., (0.2 kg) and accounting for about 0.3% of his body weight.
To put the gut microbe number in a more comprehensible perspective, at a speed of counting 5 heads of microbes per second, if we could tick like a clock that has an unlimited power source, nonstop, 24/7, it would take us many more than 240,000 years (many, many lifetimes) to count just one person’s gut microbes!
How tiny are gut microbes?
Human cells have a diameter ranging from about 8 μm (1 μm, or micrometer, is equivalent to 0.000039 inches or 0.001 mm) to 120 μm, whereas gut bacteria diameters range only from about 0.5 μm to 5 μm. By comparison, the diameter of an average human hair is about 25 μm (0.000984 inches or 0.0025 cm) to 50 μm.
Genes We Lack
Gut microbes have genes that we lack, so they are able to perform tasks that we can’t. Humans have about 20,000 genes, and an individual’s genome is fixed for life. The gut microbes contain about 150 times more genes than the human genome. But our gut microbiome changes depending on what bacteria species are residing in our gut at a given time.
At the beginning of this year, a new study added 1,520 reference genomes from cultivated human gut bacteria to the existing human gut bacteria reference genome databanks. In total, scientists have discovered that as many as 2,000 different bacteria can thrive in the human gut.
A much smaller subset of these gut bacteria, about 50–160, live in any one individual. While the species of gut microbes are not identical in all individuals, studies show that 75 species were commonly found in 50% of healthy study participants, and 57 species were common in 90% of them. So the roughly 50–100 gut bacteria species that are found in many healthy individuals constitute a typical microbiome.
However, scientists have not consented to one simple, absolute (or standardized) definition of what a healthy, normal, human gut microbiome is. There are many factors and variables that impact an individual's gut microbiome (see below, Why do people have different gut microbes?). Scientists have proposed different approaches to characterize a normal, healthy gut microbiome.
For example, suggestions have been made of a core microbiome composed of the same abundant microbes present in all individuals. Several different signature compositional patterns of microbes, termed enterotypes, have also been proposed but remain controversial. Others have tried to characterize a healthy gut microbiome by looking at its healthy functions.
The current trend has moved toward looking at the functions and interactions of whole microbial communities as a complex ecosystem in which a range of microbes interact with each other, rather than the presence of specific gut microbe species or microbial composition.
Our gut microbiome is composed of both potentially beneficial and potentially harmful bacteria species. In healthy individuals, beneficial ones are dominated by the Lactobacillus and Bifidobacterium groups. Harmful bacteria include the groups Clostridium and Staphylococcus.
Even the species common to many people may be present in different amounts or in different ratios in different individuals. In addition, an individual’s composition and function of gut microbes will vary over time depending on many health and lifestyle factors. But individuals tend to remain more like themselves than others over time.
Factors contributing to individual gut microbiome differences in composition and in function include:
- Mode of delivery and exposure to mother’s microbes
- Feeding type in infancy (breast milk, formula)
- Diet
- Immunity
- Health status or illness
- Medication
- Exposure to antibiotics
- Geographic location (latitude, altitude, climate, local diet tradition)
- Stress and emotional state
- Age
- Use of prebiotics/probiotics
- Living arrangements and household sharing
- Physical activity
- Genetic makeup
- Smoking
- Gender
- Stool consistency

All of these factors contribute to the development and shaping of our gut microbiome and continue dynamically throughout our lifetime.
Diet, antibiotic exposure, and geographic location are environmental factors that exert profound impact on both the composition and short-term and long-term function of our gut microbiome.
For example, researchers show in animal studies that diets low in microbial-accessible carbohydrates (complex carbohydrates) and high in simple sugars result in the loss of gut microbial diversity and the extinction of specific bacterial groups.
This loss is compounded over generations, influencing the ability of gut bacteria to be transferred from parents to their offspring. The transgenerational loss of diversity cannot be remedied or corrected by diet alone. Simply restoring fiber consumption is not enough to reverse this effect.