Defense from the Inside Out
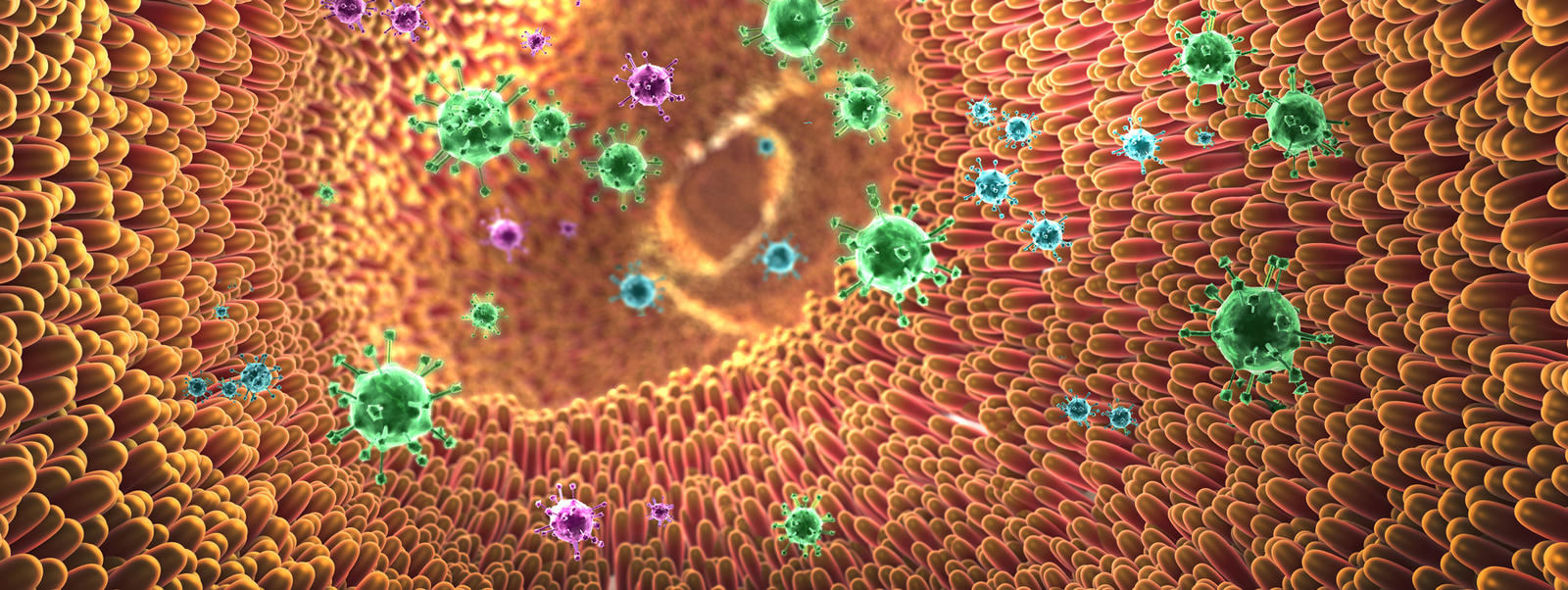
How our gut microbiome is connected to our immune system.
by Lillian So Chan with Manny W Radomski, PhD
How our gut microbiome is connected to our immune system.
by Lillian So Chan with Manny W Radomski, PhD

Our world is full of colors. Lights of different wavelengths are reflected off visible surfaces and our brain shades and frames them as pictures. Colors are seen from the inside out.
Our environment is filled with elements that nurture and inspire life: water, air, trees, and fragrant flowers. Elements that are detrimental to health and threatening to our survival, such as pathogens that cause infections and allergens that cause allergies, are also lurking everywhere.
To simultaneously defend our bodies from harmful foreign substances or invading microorganisms and permit the entry of nutrients, our immune system has evolved into a complex, highly specialized, and effective internal defense system. An effective immune system is essential to life and health. And it is intimately related to our gut with its resident gut microbes.
To paraphrase Sun Tzu, the greatest victory is one that requires no battle. By the same token, our immunity wins biggest when all is in balance, when gut and immune homeostasis have been achieved, when all fronts are peaceful, and we remain well from the inside out.
“An army marches on its stomach.”
— NAPOLEON BONAPARTE
 Skin protects us from the external environment. Likewise, the mucosa covering our digestive system protects the rest of our body from the internal passage environment running from the mouth to the anus—a moist, dark, warm environment where many pathogens from foods and drinks regularly pass through. From the time we are in the womb to the time we die, our immune system protects us. Our gut microbiome also accompanies us from before birth and until death.
Skin protects us from the external environment. Likewise, the mucosa covering our digestive system protects the rest of our body from the internal passage environment running from the mouth to the anus—a moist, dark, warm environment where many pathogens from foods and drinks regularly pass through. From the time we are in the womb to the time we die, our immune system protects us. Our gut microbiome also accompanies us from before birth and until death.
Since our gut is the most hazardous environment and the longest border that our immune system has to guard, it is, not surprisingly, our body’s largest immune organ. About 70% of our immune system is located in and around our gut, where harmful foreign invaders are most likely to attack.
Numerous studies confirm the critical role of the gut microbiome in mediating the development, education (priming), and maturation of our immune system. Our gut microbiome development is causally related to healthy growth.
The gut microbiome’s influence is not limited to the early years. It continues to actively engage all aspects of the regulation of our immune system. The health status of our gut and gut microbiome significantly impacts our immune status. Conversely, our immune status influences the composition and function of our gut microbiome.
Individuals’ immune responses vary greatly. The interplay of numerous genetic and environmental factors contributes to an individual’s immunity and susceptibility to immunity-associated disorders. Many of these same factors also contribute to our gut health and the shaping of our gut microbiome.
To effectively protect us, our immune system must recognize and correctly deal with elements that are beneficial or harmful to us. It employs various immune cells and chemical substances, such as antibodies (immunoglobulins), that can recognize and inactivate or destroy harmful substances and invading microbes.

The most important tasks of our immune system are:
When our immune system misidentifies harmless substances as harmful, becomes sensitive, or overreacts, we are susceptible to allergies. When our immune system misfires at our own healthy cells and tissues, we develop autoimmune diseases. When our immunity fails to protect us from pathogens, we become infected. When it fails to identify and remove our mutated cells, cancer can develop.
On the other hand, a strong immune system gives us a better chance of fending off infections and lowers our risk of developing allergies, autoimmune diseases, and cancer.

Our gut houses trillions of bacteria that have specifically coevolved with us to form a complex and highly diverse inner ecosystem known as our gut microbiome. The gut microbiome is essential to our survival and health because beneficial microbes perform for us essential life functions that we lack the genes to perform.
Of all the vital life functions our gut microbiome performs for our benefit, perhaps the most essential roles are to help in the development, priming, and maturation of our immune system, and in the complex mechanisms of immunoregulation (the control of immune responses).

Immune response is defense launched from the inside out. Our immune system and our gut with its microbiome affect each other to orchestrate whole-body physiology, including immune functions. Our gut microbiome is the signaling hub, integrating environmental inputs, such as diet, with immune and genetic signals to influence and regulate our immune functions. It contributes and responds to conditions in the gut in health and in diseases, providing signals critical to immune homeostasis.
Our gut microbiome's immunomodulation (regulatory) effects are not limited to the gut, but are integrated with whole-body immunity. In fact, mounting evidence shows that the composition and function of our gut microbiome influences the quality, intensity, and duration of all immune reactions. Disruption in the communication and alliance between our immune system and our gut with its microbiome contributes to complex and chronic diseases.

In numerous recent studies, our gut microbiome has emerged as a potent regulator of our immune system. It is now evident that our gut microbiome shapes our immune system and regulates and contributes to immune cell differentiation, regeneration, maturation, and activity. It is intertwined with almost all aspects of our physiology.
Our gut microbiome and immune system communicate constantly on cellular and molecular levels, influencing immune signaling and immunity-related gene expressions. The gut microbiome not only contributes and responds locally in the gut, but it also impacts organs throughout the body.
Our gut microbiome is integrated with both of the two major immune strategies in our body—regulating and significantly involved with both our innate and adaptive immunities.

We are born with innate immunity, and innate immune responses are general. The main functions of innate immunity are:
Cells of our innate immunity are located strategically at the host-microbiome interface. These cells have the ability to sense microbes or their components and metabolites, and to translate the signals into physiological and immune responses.
Our gut wall is equipped with an extensive repertoire of innate immune receptors, which are critical for recognizing whether gut microbes are friends or foes.
A network of interactions and cross talk in our gut characterizes the interdependence between innate immune strategy and our gut and gut microbiome.

Adaptive immunity is acquired and highly specific. This strategy employs different types of immune cells (such as B cells that secrete antibodies specific to a particular pathogen, killer T cells, and regulator T cells) and processes that eliminate pathogens and toxins. One of the most abundant immune cell populations in the gut comprises T cells.
Studies suggest roles for diverse species of gut microbes in regulating distinct branches of our adaptive immunity. Immune B cells and T cells play critical roles in maintaining immune homeostasis by suppressing inappropriate responses to harmless antigens and enforcing the integrity of gut barrier mucosa function.
The colonization and location of our gut microbes influence the functional diversity and the repertories of immune B cells and T cells. In the gut, these cells have location-specific and type-specific functions that are influenced by our gut microbiome.
Imbalance in the gut microbiome (dysbiosis) can induce inappropriate activity of these cells both in the gut and at distant sites, triggering various immune-mediated disorders.
Inflammation is a natural defense response of the immune system to harmful stimuli, such as pathogens, damaged cells, toxic compounds, or irritation. It is vital to life and is activated to remove harmful stimuli and initiate the healing process. However, inappropriate, dysregulated, and chronic inflammation is a common immune response underlying immune-mediated disorders such as allergic asthma, IBD (inflammatory bowel disease), MS (multiple sclerosis), and rheumatoid arthritis.

Inflammatory response initially acts locally at an injured site, but a large load of stimuli and sustained damage signals may also activate a systemic (whole-body) inflammatory response. During acute inflammatory responses, cellular and molecular immune events and interactions are usually sufficient to minimize impending injury or infection. Yet, for inflammatory responses to be beneficial, they must be controlled and properly regulated. The immune system’s efforts to activate inflammation, to halt inflammation, and to turn on healing must be well orchestrated.
Uncontrolled inflammatory responses may become dysregulated, chronic, and unresolved, contributing to a variety of chronic inflammatory diseases including obesity, type 2 diabetes, cardiovascular disease, arthritis, bowel diseases, asthma, and cancer.
In the gut setting, pathogens can release toxins to penetrate mucosal layers and manipulate gut immunity to get inside the body. The integrity of the gut wall defense barrier is critical for preventing the translocation of pathogens and toxins from the gut passage into the inner layers of the mucosa—or worse, into our blood circulation and other parts of the body.
Gut microbiome dysbiosis (imbalance), resulting from genetic and environmental factors including antibiotic use and poor diet, is associated with compromised gut barrier integrity, mucosa permeability (“leaky gut”), inappropriate immune response and/or chronic inflammation, and increased susceptibility to immune-mediated diseases such as infections, allergies, autoimmune diseases, and cancer.

“If we desire to avoid insult, we must be able to repel it; if we desire to secure peace, one of the most powerful instruments of our rising prosperity, it must be known, that we are at all times ready for war.”
— GEORGE WASHINGTON
Science is just beginning to unravel and appreciate the complexity and significance of our immune-gut microbiome interaction and communication networks. Recent studies have shown that the gut microbiome plays key roles in defending us and influencing our susceptibility to immune-mediated diseases including infections, allergies, autoimmune and inflammatory disorders.
Let’s consider the broad scope of the gut microbiome’s involvement in immune activity and regulation.

A beneficial gut microbiome
Mucus
Tight junctions on the gut wall



As you can see, the gut microbiome is hard at work identifying and responding to potential threats.

“The only source of knowledge is experience… Peace can only be achieved by understanding.”
— ALBERT EINSTEIN

Recent research data shows that infectious diseases are not just single pathogen (virus or bacteria) problems. Health or infectious disease is actually a reflection of the interplay between our immune response, our gut microbiome, and potential pathogens.
A balanced gut microbiome defends us from the inside out; however, disruption of our gut microbiome changes the overall dynamics between gut microbiome function and our immune system. Studies show that disturbing the composition and function of our gut microbiome is associated with infectious disease susceptibility as well as some disease outcomes.
As infectious disease research shifts from a single pathogen reductionist approach to understanding the dynamic and balance between gut microbiome, immune responses, and potential pathogens, we will gain greater insights into how infectious diseases can be prevented and treated. In this regard, the association between flu virus infection and the gut microbiome provides a clear, illustrative example. Recent animal and human studies show that the gut microbiome influences susceptibility to flu virus infection, the effectiveness of flu shots, and flu infection virulence.
How do the beneficial gut microbes in our digestive system collaborate with and influence our respiratory system?
Our gut and its resident commensal microbes are at the forefront of our longest line of defense against harmful viruses. It is therefore not surprising that immune-mediated diseases such as flu infection, and the effectiveness of vaccines—including flu shots—are associated with our gut microbes.

The beneficial effects of the gut microbiome against flu virus infection were first identified more than a decade ago. Since then, it has gradually become known that these defenses against flu viruses are dependent on immunoregulatory cells and factors traveling between the gut and the respiratory system via our lymphatic and blood circulations. They establish a defensive parameter against incoming infectious pathogens or allergens in the airways and lungs.
In the last few years, how the gut microbiome and its commensal metabolites exert protective effects on the respiratory system has become a research area of great interest.
One means of communication found between the gut and the respiratory system is through soluble gut microbial components and metabolites, including gut microbial-derived short chain fatty acids (SCFAs). Emerging evidence involving SCFAs has highlighted a link between the gut, the respiratory system, and bone marrow.
It seems that the protective effects of SCFAs on the respiratory system, including protection against flu infection, are mainly indirect. It is through their effects on immune cells and the subsequent recruitments of immune cells to the respiratory system that SCFAs promote lung immunity and protect against respiratory infections.
Study data suggests that SCFAs help prime immune cells in the bone marrow against respiratory system infections (including flu), limit inappropriate inflammation, and mediate and refine antiviral immune responses. Because SCFA levels in the gut and circulation are dependent on the fermentation of fiber by gut microbes, diet and SCFAs represent a promising preventative and therapeutic approach for respiratory infections.
Animal studies have identified a correlation between flu virus infection virulence and gut microbiome diversity. Furthermore, research data from recent months, in both human and animal studies, has confirmed many findings from earlier animal studies on the associations between gut microbiome and the effectiveness of the flu shot.

Seasonal flu is a serious disease that causes millions of illnesses, hundreds of thousands of hospitalizations, and tens of thousands of deaths globally every year. According to thirty-six years of the US Centers for Disease Control and Prevention (CDC) records, flu activity in the US peaked most often in February, followed by December, January, and March.
The CDC estimates that on average, between 5–20% of the US population gets the flu each year. It is estimated that during the 2018–2019 flu season, up to 42.9 million people in the US got sick with flu, there were 17–20 million flu medical visits, up to 647,000 flu hospitalizations, and 61,200 flu deaths. In Canada, there is an annual average of 12,200 flu-related hospitalizations and 3,500 deaths.
As of February 29, 2020, the CDC reported that key indicators of flu activity remain high for the current flu season. Even though the flu activity has decreased three weeks in a row, hospitalization rates remain high among children and young adults. Hospitalization rates among children under age four was at the highest recorded by the CDC compared to the same time in previous years, surpassing rates reported during the 2009 H1N1 pandemic. The highest hospitalization rate overall is among the age group 65 and older.
It is estimated that there have been 34–49 million cases of flu illnesses, 350,000–620,000 hospitalizations, and 20,000–52,000 deaths from flu in the US this flu season, from October 1, 2019, to February 29, 2020. Flu activity is expected to continue for weeks.
Although many people may encounter the same flu virus, only some of them will become infected. How well the current season’s flu can be fended off depends on how strong an individual’s immunity is, whether it is fortified with a flu shot, and how effectively the flu shot primes an individual’s immunity.

The flu shot consists of inactivated virus strains that educate the immune system to protect us when we encounter the active, disease-causing flu virus. Flu vaccines must be updated annually because flu viruses mutate rapidly.
According to the US National Foundation for Infectious Diseases, during the 2017–2018 flu season, the flu shot prevented an estimated 7 million flu illnesses, 109,000 flu hospitalizations, and 8,000 flu deaths. About 45% of American adults and almost 63% of children got a flu shot during the last flu season.
However, the flu shot’s effectiveness only ranged from 30–60%. Why?
How well the flu vaccine matches the major circulating flu strains is just one factor. A flu vaccine’s effectiveness also depends on its ability to stimulate the immune system and the quality and duration of the individual’s immune response to it. The recipient’s age, sex, nutrition status, general health, genetics, and prior exposure and infections, among other factors, all contribute to the efficacy of a flu shot.
Another significant factor that emerged in recent years is our gut microbes.
Studies on mice strongly indicate that gut bacteria have a significant positive effect on the efficacy of a number of different vaccines, including flu vaccines. Studies from the last two years report that not only is the effectiveness of the flu shot linked to the gut microbiome, but the gut microbiome may determine the effectiveness of the shot.
The first human study on the role of the gut microbiome in shaping immune response to flu shot was reported just a few months ago. The researchers found that antibiotics hindered immune response to a specific strain of virus in the flu shot that was derived from three different strains of viruses.
Antibiotic-treated participants produced fewer antibodies (and therefore had reduced immune protection) in response to the flu shot compared to those who did not take antibiotics. Those treated with antibiotics also experienced cellular and gene transcriptional changes in their immune system, which indicates a pro-inflammatory state.

On the other hand, some review studies on the use of probiotics and flu shot effectiveness found that probiotics can enhance antibody response to flu vaccine and induce greater protection. Other studies found that the longer an individual took the probiotics, the greater their response to their flu shot. Seniors who used probiotics also showed enhanced flu shot response. Another review study found that ingestion of prebiotics for sixteen weeks resulted in increased response to flu vaccine. In general, the best response to flu shot for individuals using probiotics and prebiotics was experienced by healthy older adults, followed by healthy young- to middle-aged adults.
Taken together, studies find that the gut microbiome exerts various effects on our immune responses to the flu shot, not only by interacting directly with immune cells, but also by regulating the availability of important microbial products, including metabolites such as SCFAs and bile acids. Findings also show that:

“The best defensive is the winning offensive… a champion general wins (in defending) before entering into war.”
— Sun Tzu

Most gut microbes exert several specialized, complementary, and redundant immune-regulation and gene expression transcriptional (turning genes on or off) effects on us.
A sufficiently large community of species with diverse immunologic input allows for buffering in case certain community members are lost, providing consistency in the microbiome’s ability to generate immune regulation impact. Microbial diversity in the gut also ensures a balance among species in the community, stabilizes the immunologic changes they induced, and therefore optimizes the overall health of the gut microbiome and our general health.
Even though the interplay of genetic and environmental factors contributes to the composition and function of our gut microbiome, there is strong evidence that environmental factors, especially diet and the use of antibiotics, predominantly shape our gut microbiome. In this regard, diet is a well-established driver of microbiome composition and function, and a diet high in fiber is linked to gut microbiome diversity. Gut microbial production of short chain fatty acids (SCFAs) in the fermentation of fiber reduces inappropriate inflammation and promotes immune health.
The use of probiotics and/or prebiotics has been shown to improve gut health, enhance commensal gut microbial diversity, boost immune defense, and reduce infection-related damage, such as flu virus-related damage to the lungs.
In studies, the diversity of our gut microbiome is increasingly regarded by scientists as an indicator of health in a variety of contexts, whereas many disease states are associated with low or decreased diversity. Emerging research shows that immunity seems to be integral to the maintenance of gut microbiome diversity. The balance and diversity status of our gut microbiome is impaired by a weak or compromised immune system.

A healthy gut and balanced gut microbiome are necessary for immune homeostasis and overall health. Our every breath and movement takes worlds of effort—the combined hard work of our trillions of cells with their genes, and our trillions of gut microbes and their genes. Our immune system and our gut microbiome are interdependent, intimate, working allies that defend us from the inside out. We can never know how many times our inner, unseen defenses have kept us safe from the potential harm lurking in every corner of our external and internal worlds.
General Douglas MacArthur once remarked that, “A general is just as good or just as bad as the troops under his command make him.” A champion general would be appreciative and proud of the military forces under him/her and take mindful care of them. Why wouldn’t we feel the same about our gut-immunity defense alliance, and be mindful of our gut and gut microbiome health?

Curious about how well your gut is supporting your immune system? The Ixcela test measures how well your gut is supporting five ares of health including Gastrointestinal Fitness, Emotional Balance, Cognitive Acuity, Energetic Efficiency, and Immuno Fitness.

 |
Lillian So Chan is the founding editor of WellnessOptions, a print magazine and website, and author of the book WellnessOptions Guide to Health published by Penguin Books. With over thirty years of experience in journalism and editing, Lillian has established unique editorial directions for several award-winning publications. She has worked for Maclean’s, Canada's largest news magazine, and served as a Governor and Deputy Chairperson of the Board of Governors at the Simon Fraser University, British Columbia, Canada. |

|
He served as Scientific Advisor to the Chief of Air Staff, Defence Canada; Board Director of the Canadian Defence Research and Development Executive Committee; member on the NATO Research and Technology Agency’s Human Factors and Medicine Panel. He is the former Editor-in-Chief of the Undersea Biomedical Research Journal and serves as a referee for the Aviation, Space, and Environmental Medicine Journal. He has published on diving and aerospace medicine, human performance and protection, stress endocrinology, sleep, tropical medicine, and circadian disorders. Manny is a co-editor of WellnessOptions. |
|
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Interested in learning more about Ixcela? Learn more about Ixcela’s Internal Fitness Test to help you optimize your health.
|